Katrina M. Ward, Dr. Renee S. MacPhee
Ward KM, MacPhee RS. Investigating Complementary and Alternative Medicine Use Among Seniors. UBCMJ. 2015: 7.1 (21-24).
Abstract
Objectives: Complementary and alternative medicine (CAM) is used regularly by 70 % of Canadians, but when compared to younger users of CAM, seniors tend to use it less frequently. Using a phenomenological approach, this study sought to explore the attitudes and beliefs of seniors towards the use of CAM.
Methods: This qualitative study used either in–depth personal interviews or focus group interviews as the primary means of data collection. Participants in the study were individuals who had either used CAM in the past, or who were currently using CAM.
Results: Participants described that they would use conventional treatment for pathological disease, but would prefer to use CAM in certain circumstances as it was perceived to be a more natural approach. Exercise was also described as a form of CAM. Deterrents for CAM use include limited scientific evidence, cost, and the attitudes of others (e.g., physicians, the public).
Conclusion: Participants felt that they had positive experiences using CAM as an adjunct to conventional medicine, and felt that they had no personal barriers to accessing CAM. A major deterrent of CAM use was the limited scientific evidence, while minor factors included cost and the attitudes of others. Open discussion about CAM use should take place between physician and patients.
Introduction
Complementary and alternative medicine (CAM) typically includes therapies or treatments that are not considered mainstream in North America. More specifically, CAM is defined as modalities that are not extensively taught in North American medical schools and are not widely used in North American healthcare institutions (i.e., hospitals or medical clinics).[1] CAM is often used instead of, or in conjunction with, conventional treatment modalities (e.g., surgery, pharmaceuticals, etc.). According to the Public Health Agency of Canada, it is estimated that more than 70 % of Canadians regularly use at least one form of CAM.[2,3] CAM can include acupuncture, chiropractic care, massage therapy, yoga, diet–based therapies, naturopathy, homeopathy, osteopathy, and herbal remedies.[2]
The results of previous research suggest that CAM is used more often by individuals who have chronic health problems because it reportedly gives them a sense of control over their health, and may improve quality of life.[2,4,5] In addition, the literature suggests that some of the factors that influence the use of CAM include dissatisfaction with traditional treatments [2,4,6,7,8] , personal attitudes [2,4,6], culture [5], and a holistic concept of health.[6] While as many as 90 % of seniors (i.e., individuals aged 65 years or older) live with at least one chronic disease [9] they tend to be less well represented among users of CAM, particularly when compared to younger individuals.[7] To date, there is limited research on the use of CAM by seniors, which may be in part due to the potential for confounding effects with conventional treatments, and possible loss of follow–up due to death or illness.[8]
This study was designed to explore the attitudes and experiences of seniors with their use of CAM. This research also aimed to identify barriers that affect the use of CAM in seniors.
Materials & Methods
Data were collected via in–depth personal or focus group interviews. In order to be eligible to participate in the study, participants had to be 65 years of age or older and either previous or current users of CAM. Participants were recruited using one of two approaches: 1) purposeful convenience sampling, wherein prospective participants were known to the researcher; or 2) self-selection wherein posters and recruitment speeches at senior’s centres in Kitchener–Waterloo were used to inform prospective participants, who contacted the researcher directly via email or telephone. At the end of three weeks, a total of 16 participants had enrolled in the study; at this time, all recruitment posters were removed.
Interviews took place at a location that was convenient for both the participants and the researcher. Prior to the start of each interview, the researcher ensured that each participant met the inclusion criteria, and either a verbal or written informed consent was obtained. A standardized set of seven open–ended questions was used to guide each of the interviews. Key questions included:
- Do you have any experiences, past or present, with complementary and alternative medicine?
- Do you have any reasons why you chose/choose to use complementary and alternative medicine?
- What are the barriers that affect your access or decision to use complementary and alternative medicine?
All interviews were audiotaped. During the interviews, the researcher took field notes that identified general observations and key phrases. Each interview was transcribed verbatim, and with identifying information removed to ensure confidentiality, each participant was sent his/her transcript and asked to review it in order to ensure the accuracy of the information.
Approval for this study was obtained from the Research Ethics Board at Wilfrid Laurier University. This study was done as an undergraduate thesis project. The participants did not receive financial compensation.
Analyses
Using a phenomenological approach, the data analysis sought to examine the lived experiences of participants. Because the study was evaluating the subjective experiences of more than one individual to find meaning in their lived experience, the phenomenological approach was the most suitable approach to analyze this qualitative study.[10] The transcript was initially examined for broad, common, recurring themes. The broad themes were further broken down into sub–categories following subsequent detailed readings.[11] Concepts that were identified by eight or more of the participants were described as a major theme. Furthermore, concepts that were articulated by three or more of the participants were identified as sub–themes. The transcripts were reviewed to the point where no further themes could be identified.
Results
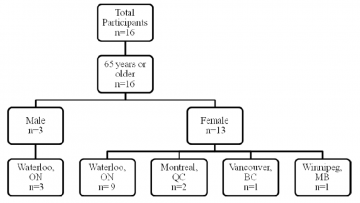
16 participants who met the inclusion criteria were included in the study. Three participants were recruited using the convenience sampling technique; the remainder of the participants (n=13) self–selected to participate in the study. The participants consisted of three men and 13 women. All participants were aged 65 years or older: 11 participants were between 65 and 74 years of age; two participants were between 75 and 84 years of age; and three participants were 85 years of age or older. The mean age of participants was 74.5 years. 12 participants resided in the Kitchener–Waterloo area, while the remaining four participants lived outside the province of Ontario. The characteristics of the participants are provided in Figure 1.
Seven in–depth personal interviews were conducted in this study. Four of the interviews were conducted via the telephone due to geographical location of the participants relative to the researcher; the remaining three interviews were conducted in person.
Three focus group interviews were conducted. In each focus group, the number of participants ranged from two to four in each interview.
Participants had experiences with a wide range of alternative therapies, including yoga (n=12), massage therapy (n=9), tai chi (n=8), chiropractic care (n=7), acupuncture (n=6), osteopathy (n=4), and naturopathy (n=4). Other forms of CAM that were less frequently utilized included herbal remedies and natural health products (n=3), vitamins and probiotics (n=3), spiritual healing (n=2), homeopathy (n=1), aromatherapy (n=1), biofeedback (n=1), reflexology (n=1), and energy healing (n=1). All of the participants were using CAM in addition to traditional medical treatments.
The length of interviews ranged from 20 minutes to 90 minutes. Personal interviews ranged from 20 minutes to 36 minutes, taking on average 22 minutes to complete. Focus groups ranged from 25 to 90 minutes, taking on average 75 minutes to complete.
Themes
In order to maintain the privacy of the participants, abbreviations to denote participation in a focus group or personal interview were used in place of their personal identifiers (i.e., first and last names). Each of the three focus groups (FG) was assigned a number (e.g. FG1; FG2; FG3); personal interviews (PI) were numbered according to the participant that was interviewed. Each participant was assigned a number and identifiers were removed. A slash was used to separate the type of interview that was conducted and the number assigned to the participant. For example, FG2/8 described a quote by Participant 8 in focus group 2. A statement made by Participant 11 in a personal interview is denoted PI/11.
Major Theme 1: Participants tried to use CAM as an alternative to only prescription medications
The first major theme identified, which was identified by the vast majority of participants, was that CAM was used as an alternative to conventional medicine. Participants felt that they were responsible for their own health, and that CAM gave them more control over their health outcomes.
“I’d much rather try a natural thing than have a medication. I don’t like taking medications; unfortunately at my age you have to.” (FG2/8)
“…I tend to be a bit skeptical about medication and fixing symptoms and this is happening to your body for a reason, you know, what is it?” (FG1/5)
Sub–theme 1: Physical activity was considered to be a form of CAM by participants
A sub–theme that emerged was that many of the participants considered exercise to be a form of CAM. These participants included physical activity as a way of promoting good health, preventing disease, and speeding up recovery of musculoskeletal injuries:
“I consider any sport, any physical activity, to be something that is health, uh, promoting, and health maintaining.” (FG3/14)
“For example, I’ve been running for 42 years. I consider that medicine.” (FG3/16)
“That’s a theme that I am seeing more and more in medicine, and that is that our bodies were made to move.” (FG3/16)
“I maintain my heart condition is better because I exercise.” (PI/11)
Major Theme 2: Seniors’ decision to use CAM is influenced by several factors
All but one of the participants expressed that they did not feel that they had any personal barriers to accessing CAM. Factors that the participants felt influenced the use of CAM among seniors are expressed as sub–themes below:
Sub–theme 1: The limited regulation and scientific evidence related to CAM is a major factor that influences the use of CAM
Participants felt that one of the factors that influenced the use of CAM among seniors was the lack of regulation and scientific evidence. This theme was very prevalent in the third focus group interview, where all four of its participants felt that this deterred them from using certain alternative therapies, such as reflexology, naturopathy, or homeopathy:
“Many of those haven’t been— they aren’t regulated so I wouldn’t really go for them.” (PI/1)
“I don’t— well, I just don’t think that their remedies are as effective as a medical doctor… I don’t think they’re scientifically proven, and I don’t think they’re as effective. I think there’s a lot of placebo effect.” (FG3/16)
The importance of scientific evidence was made evident by participants who acknowledged that they would still seek conventional treatment for a pathological illness rather than using alternative medicine.
“As far as osteopenia is concerned, I know certainly the drugs available are very beneficial, so I would use them. Were I to have an infection, I would feel that would need to be treated medically… I do believe that there are some true medical issues that need to be dealt with, you have to deal with them.” (PI/12)
Sub–theme 2: Cost as a deterrent for ongoing CAM use
Participants described cost as a factor that prevented people from continuing their use of CAM beyond what they felt was directly necessary for their healing process. Participants indicated that cost would not stop them from going for an initial visit, but if treatment were to be ongoing they might feel that CAM was too costly.
Sub–theme 3: External factors affect the use of CAM
This sub–theme was a reflection of the belief that the attitudes of the public, physicians, and the patient–physician relationship were all factors in seniors’ decisions to use CAM. Some participants felt that there was public judgment when deciding to use CAM. On the other hand, several participants expressed that there tends to be more acknowledgement of CAM now than there used to be. Participants who felt that they had a stronger patient–physician relationship were more comfortable bringing up their use of CAM with their physician.
Discussion
This study explored the use of CAM by seniors through the use of in–depth personal interviews and focus group interviews. The study highlighted that because CAM has limited scientific evidence, seniors tend to seek conventional treatment for a pathological illness rather than using alternative medicine. With respect to musculoskeletal injuries or maintaining general well–being as they aged, some of the participants preferred to use CAM over a conventional therapy. This is consistent with the research literature that suggests that CAM is most often used for back and neck pain, followed by stress and anxiety.[2] Older adults could benefit from an open discussion with their physicians about using CAM as an adjunct to conventional therapy when considering treatment options.
An unexpected and very significant theme that emerged pertained to the belief that physical activity is very relevant in personal health promotion and maintenance. This finding was strongly expressed by 15 of the 16 participants in the study. Physical activity is supported in the literature as being a factor in the prevention and management of numerous chronic diseases, including diabetes, obesity, hypertension, and heart disease.[12] Furthermore, when looking at the traditional definition of CAM, self–directed daily exercise was not often included as a form of alternative therapy. A study done by McFadden et al. suggests that individuals who believe in the principles of CAM report doing more aerobic exercise than those who are not strong believers in CAM (p=0.041) [6], and that CAM users are more likely to engage in a healthy lifestyle than nonusers.[13] One participant expressed this theme by saying, “[for] example, I’ve been running for 42 years. I consider that medicine” (FG3/16). Self–directed physical activity, such as performing yoga at home, running, or walking, was part of the daily routine of more than half of the participants. These activities may also be less costly and more accessible than some of the other alternative therapies such as acupuncture. This finding may suggest that physical activity should be acknowledged as part of the definition of CAM and supports that physical activity should be a central part of the lives of seniors.
There were several limitations to this study. The first is that the study had a small sample size (n=16). This was due largely to the time constraints associated with an undergraduate thesis. Despite this, interviews were conducted to the point of saturation.[14] Another limitation is that the sample itself may not be representative of the senior population at large. Reasons for this may include: the majority of the seniors self–selected for the study (a possible form of recruitment bias because these individuals may have been in a better financial position to engage in CAM services); participants were predominantly female (female n=13; male n=3); participants had positive experiences with CAM such that they wanted to share and promote CAM; all the participants were residents of a suburban or urban area rather than a remote or rural community (the literature search suggests higher rates of CAM use in rural communities as compared to urban communities[15,16]); and only seniors who had used CAM were recruited due to time constraints.
Conclusion
In summary, participants felt that by using CAM they were actively taking control of their health needs. Overall, seniors did not feel that they had any barriers in their access to CAM, though in general, factors such as cost, attitudes, and regulation would affect their decision to use more alternative therapies. It was encouraging to hear that physical activity was viewed as such a positive factor in maintaining health and well–being of seniors, and some participants considered physical activity to be a form of CAM.
Future research could compare senior participants who do not use CAM with those who do in order to determine whether there are any differences in attitudes or beliefs, or perceptions of barriers. In addition, research could also examine how the use of CAM differs in rural and urban settings or among seniors of different ethnicities.
Disclosures
The authors did not have any conflicts of interest that would affect this research.
References
- Williamson AT, Fletcher PC, Dawson KA. Complementary and alternative medicine use in an older population. J Gerontol Nurs. 2003 May;29(5):20‑8.
- Esmail N. Complementary and alternative medicine in Canada: trends in use and public attitudes, 1997‑2006. Public Policy Sources. 2007 May;87.
- Complementary and Alternative Health [Internet]. Canada: Government of Canada; 2008 Apr 1 [cited 2015 Jan 25]. Available from: http://www.phac-aspc.gc.ca/chn-rcs/cah-acps-eng.php.
- Williams AM, Kitchen P, Eby J. Alternative health care consultations in Ontario, Canada; a geographic and socio–demographic analysis. BMC Complement Altern Med. 2011 Jun 22;11(47).
- Loera J, Reyes-Ortiz C, Kvo Y-F. Predictors of complementary and alternative medicine use among older Mexican Americans. Complement Ther Clin Pract. 2007 Nov 1;13(4): 224‑31.
- McFadden KL, Hernández TD, Ito TA. Attitudes toward complementary and alternative medicine influence its use. Explore (NY). 2010 Nov-Dec;6(6):380‑88.
- Adams J, Lui C-W, McLauglin D. The use of complementary and alternative medicine in later life. Rev Clin Gerontol. 2009 Nov;19:227‑36.
- Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012 Sep;11(3):187‑203.
- Government of Canada – Action for Seniors Report [Internet]. Canada: Government of Canada; 2014 Jul 3 [cited 2015 Jan 25]. Available from: http://www.seniors.gc.ca/eng/report/index.shtml#tc6.
- Creswell JW. Qualitative inquiry and research design: choosing among five approaches. California: Sage Publications; 2006.
- Patton MQ. Qualitative research & evaluation methods. 3rd ed. Thousand Oaks, California: Sage Publications, Inc; c2002. 598 p.
- Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports. 2006;16(Suppl. 1):3‑63.
- Nahin RL, Dahlhamer JM, Taylor BL, Barnes PM, Stussman BJ, Simile CM, Blackman MR, Chesney MA, Jackson M, Miller H et al. Health behaviors and risk factors in those who use complementary and alternative medicine. BMC Public Health. 2007 Aug;7(217).
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006 Feb;18(1):59‑82.
- Adams J, Sibbritt D, Lui C-W. The urban–rural divide in complementary and alternative medicine use: a longitudinal study of 10,638 women. BMC Complement Altern Med. 2011 Jan;11:2.
- Meurk C, Broom A, Adams J, Sibbritt D. Rurality, mobility, identity: women’s use of complementary and alternative medicine in rural Australia. Health Place. 2013 Mar;20:75‑80.
Ward KM, MacPhee RS. Investigating Complementary and Alternative Medicine Use Among Seniors. UBCMJ. 2015: 7.1 (21-24).